Renal Calculi
Once there were two patients in our surgery outdoor. They came with the same problem with haematuria; though one have severe radiating pain in loin to groin but the other patient didn’t show that types of symptoms.
After history taking and physical examination both were asked to undergo X- ray and Ultrasonogram of KUB region.
After a while, we got their results and learned briefly about ‘Renal Calculus’.
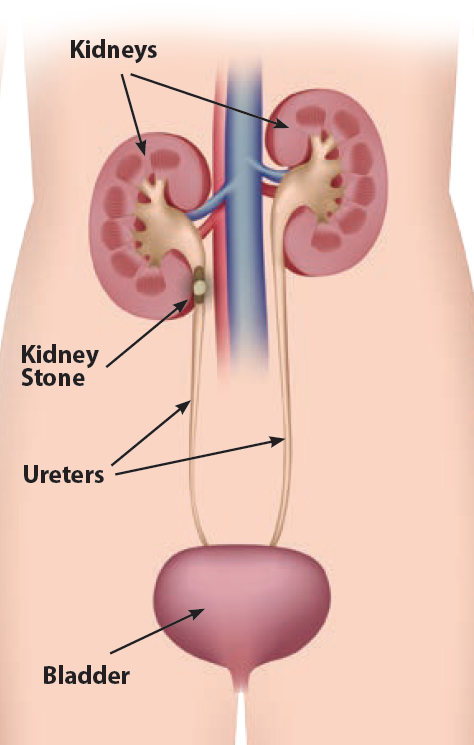
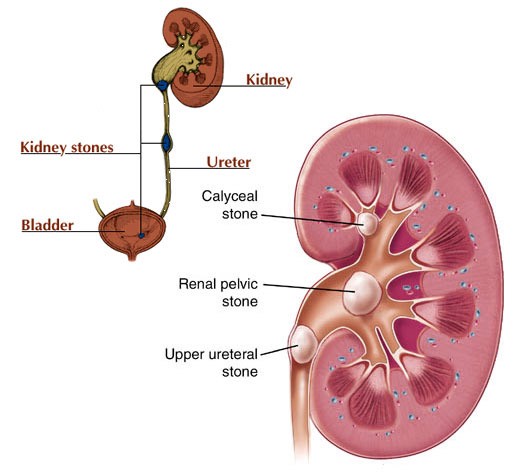
Kidney stones are also known as ‘Renal Calculus’ or ‘Nephrolith’, are hard deposites of mineral amino acid salts in the inner surface of the kidney. It may grow to sufficient size; they can cause blockage of the ureter.
If the stone is in anywhere in the Urinary system then it is called ‘Urolithiasis’.
Risk factors :-
There are many causes which are classified into following groups:
– Idiopathic urolithiasis ( It is produced by concentrated urine as consequences of dehydration or impairment of inhibitors that prevent crystallization in urine e.g. Mg, pyrophosphate, glycosaminoglycan, nephrocalcin etc. Here Tamm- Horsfall protein is a kind of substance which has a role in inhibiting formation of crystals and also has some physiological effects.)
– Hypercalcaemia ( Main reasons are
° Primary hyperparathyroidism
° Vitamin D ingestion
° Milk Alkali Syndrome
° Sarcoidosis etc)
– Hypocitruria ( As citrate binds with calcium & inhibits the formation of calcium salt.)
– Renal tubular acidosis
a) Hypercalciuria ( Most common metabolic abnormality that causes calcium stone formaltion. It is due to impaired renal tubular reabsorption of calcium.)
b) Hyperoxalouria ( Increased oxalate excretion due to defect in liver metabolism or heavy diet or oxalate rich food like rhubarb, spinach, chocolate, nuts, beer etc)
– Cystinuria ( It’s an Autosomal Recessive disorder. Cystine stones are often multiple and very hard.)
– Infection ( Due to UTI, Vesicourethral reflux or Obstructive uropathies different bacteria like Proteus, Klebsiella creates alkaline environment and form stone with Magnesium Ammonium Phosphate which form stone of ‘Staghorn’ pattern.)
– Obstruction and stasis
– Medullary sponge kidney
– Urinary diversion
– Drugs e.g. Acetazolamide, Allopurinol, Thiazide diuretics etc.
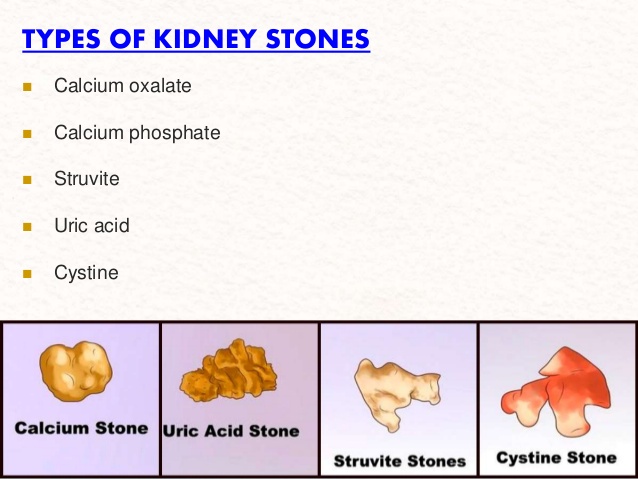
Types of renal stones :-
– Calcium stones
° Calcium oxalate stones ( about 80%, decreased pH and black or dark brown in colour. )
° Calcium phosphate stone ( about 5 – 10%, increased pH and dirty white in colour )
– Uric acid stones ( about 5 – 10% with constantly decreased pH and yellow or red brown in colour)
– Struvite stones ( about 10-15% with increased pH and dirty white in colour)
– Cystine stone ( about 1 – 2% and pink or yellow in colour)
– Xanthine stone which is rare
Stones which are radiopaque :-
– Calcium stones
– Cystine stones
– Xanthine stones
Stones which are radiolucent :-
– Uric acid stones
Sign symptoms :-
– Asymptomatic ( if stone is less than 5 mm and it might be seen while doing other investigations to evaluate other diseases. )
– Symptomatic
° Fixed renal pain : Dull aching constant pain in the loin and radiates to hypochondriac region.
° Renal ureteric colic : Acute colicky pain starts in the loin and radiates to the groin.
° Haematuria : Due to irritation by the stone.
° Pyuria : Due to associated infection may present with Hydronephrosis or Pyonephrosis.
° Diaphoresis (sometimes)
Diagnosis :-
– Urine R/M/E
– Imaging ( X-ray, IVU, CT scan of KUB region)

Prevention :-
– Proper hydration
– Ingestion of potassium citrate to avoid crystallization of stone
– Taking proper measure for infections
– Avoid stone forming foods like chocolate, rhubarbs, spinach, colas etc
Treatment :-
– Analgesic for Anti spastic and Anti inflammatory medications e.g Ibuprofen, Naproxen, Acetaminophen etc to relief pain.
– Medical therapy by Alpha- adrenergic blocker & Calcium channel blocker e.g Tamsulosin, Nifedipine etc that allows dialation of the vessels & facilitates stone for passing.
– Calculus removal :
° Non invasive procedure i.e Shockwave Lithotripsy by which the stone is broken up and pass out spontaneously when it is less than 1 cm.
° Invasive procedure i.e surgery and stent placement by Uroscope if the stone is larger than 1 cm.
References:
- Bedside Clinics in Surgery by Makhan Lal Saha
- Bailey and Love’s Short Practice of Surgery (27th edition)
- www.mayoclinic.org
4.www.health.harvard.edu
Fariha Bintay Amin (Nodi)
Institution of Applied Health Science, Chittagong.
Session: 2015-2016